Abstract
Introduction: Adenosine, an autacoid and metabolite of ATP, has been known to have anti-platelet properties. Of the 4 adenosine receptors, both A2A and/or A2B have been implicated in adenosine-mediated anti-platelet properties, while the roles of A1 and A3 have not been clearly defined in humans. In addition, previous studies show that A2A/A2B on platelets are G-Protein Coupled Receptors and are coupled to a stimulatory G-protein that activate adenylyl cyclase and subsequently increase intracellular cAMP. An elevation of cAMP in platelets inhibits aggregation. In this study, we set out to determine which adenosine receptor subtype leads to inhibition of platelet aggregation, and change in intracellular cAMP.
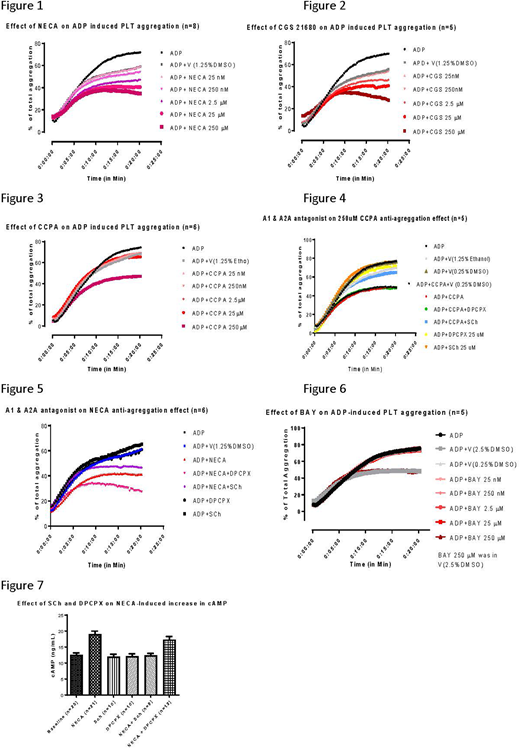
Materials and Methods: Platelet-rich plasma (PRP) was isolated from whole blood of human volunteers, and centrifuged at 200g for 10min. Light transmission aggregometry was performed by 100uM ADP with or without NECA (non-specific AR agonist), CCPA (A1 AR agonist), CGS 21680 (A2A AR agonist), BAY 60-6583 (A2B AR agonist), DPCPX (A1 AR antagonist), Sch 58261 (A2A AR antagonist), GS 6201 (A2B AR antagonist), and MRS 1220 (A3 AR antagonist). Cyclic AMP was extracted from 100ul of PRP after adding 1ml of EtOH, 10mM ammonium formate, with 10ug/ml cGMP-Br as an internal control, and measured by liquid chromatography/ Tandem Mass Spectroscopy (Quantiva, ThrermoFisher).
Results: ADP-induced platelet aggregation was inhibited in a dose dependent manner by the non-specific adenosine agonist, NECA (Figure 1). This inhibition of platelet aggregation was likely mediated by A2A receptor as the specific A2A receptor agonist had a similar effect (Figure 2). Furthermore, A2A antagonist blocked the effects of NECA (Figure 5). Stimulation of A1 receptor had no effect on the ADP-induced platelet aggregation, except at the highest concentration (250 µM), and is likely due to its non-specific effect on A2A AR (Figures 3 and 4). Blockade of A1 enhanced the effects of NECA (Figure 5). This suggest that A2A and A1 may have opposing roles for control of platelet aggregation. Stimulation of A2B receptor, had no effect on ADP-induced platelet aggregation, except at the highest concentration (250 µM), which was likely due to the non-specific vehicle effects (2.5% DMSO, Figure 6). Blockade of A2B receptor had no effect on NECA, while A3 blockade showed slight inhibition on NECA's anti-platelet effect (data not shown). NECA inhibition of platelet aggregation was likely due to elevation of intracellular cAMP as incubation for 5min with NECA stimulated intracellular cAMP (Figure 7). This effect was blocked by A2A, not by A1 antagonist.
Conclusion: Our results support previous findings that adenosine receptor A2A mediates adenosine-induced anti-platelet properties in human platelets. Adenosine and its analogs inhibit platelet aggregation to the natural stimulus, ADP. The mechanism appears to be due to elevation in intracellular cAMP. We did not find evidence that A2B played a significant role in platelet aggregation. A1 and A3. however, demonstrated modulatory effects that has not been previously described.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal